The FDA wants to pull common cold and flu medications from drugstore shelves after studies found the main ingredient was useless in relieving symptoms.
The agency proposed on Thursday discontinuing the use of phenylephrine – an ingredient in common medications like Vicks Sinex, certain types of Sudafed and Benadryl – in nonprescription products because it ‘is not effective’
The FDA began reviewing the use of phenylephrine in March 2023 and concluded it was no more effective than a placebo when taken orally in a pill.
When metabolized in the gut, phenylephrine can’t reach the bloodstream in sufficient levels, rendering it useless in providing relief.
Dr Patrizia Cavazzoni, director of the FDA’s Center for Drug Evaluation and Research (CDER), said in the agency’s notice: ‘It is the FDA’s role to ensure that drugs are safe and effective.
‘Based on our review of available data, and consistent with the advice of the advisory committee, we are taking this next step in the process to propose removing oral phenylephrine because it is not effective as a nasal decongestant.’
The proposed order only applies to the active ingredient phenylephrine, which is sold under brand-name products.
However, sometimes phenylephrine is used in products alongside other drugs and the FDA said it ‘does not affect how other active ingredients work to treat the symptoms for which they are intended.’
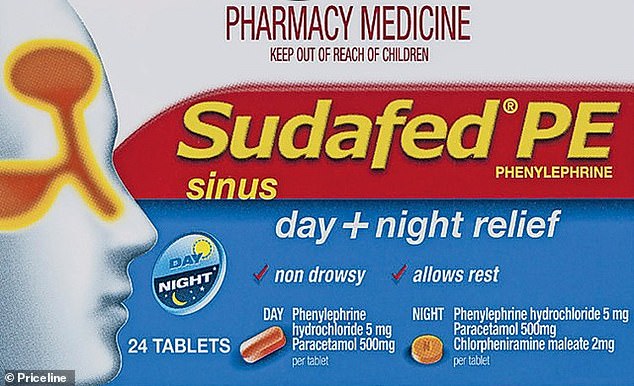
Common active ingredients phenylephrine is used with include acetaminophen – sold as a pain reliever – diphenhydramine – sold as an antihistamine – and dextromethorphan – sold as a cough suppressant.
This is only a ‘proposed order’ and will not have an immediate impact on the medications.
Only a ‘final order’ will affect the products sold, which could have a major impact on the $1.8billion in sales generated by these drugs.
The FDA added: ‘The proposed order is based on effectiveness concerns, not on safety concerns.’
The proposal is based on ‘a comprehensive review of all available data on the safety and efficacy of oral phenylephrine,’ which dates back three decades when the drug was first thought to be effective as a decongestant, as well as more recent research.
Last fall, the FDA’s Nonprescription Drug Advisory Committee met to discuss the ‘Generally Recognized as Safe and Effective’ (GRASE) status of phenylephrine.
Based on new data, it unanimously concluded ‘current scientific data do not support… phenylephrine’s effectiveness as a nasal decongestant.’
The FDA noted, however, that its conclusion only applies to phenylephrine taken orally, not intranasally in common nasal decongestants.
Scott Melville, the president and CEO of the Consumer Healthcare Product Association (CHPA), which represents manufacturers and distributors of over-the-counter drugs, said in a statement the group was ‘disappointed in the FDA’s proposal.’
He stated: ‘[Phenylephrine] is the only oral [over the counter] decongestant available without purchase restrictions and is included in numerous [over the counter] cough and cold medicines labeled with a decongestant claim.
‘Consumers need options for self-care, and freedom of choice for self-care is a core attribute of our nation’s healthcare system. [Phenylephrine] should remain an available option for consumers, because Americans deserve the option to choose the safe and effective [over the counter] medicines they prefer and rely on.’
Phenylephrine became exceedingly popular in the mid-2000s when the federal government imposed new restrictions on purchasing pseudoephedrine, an ingredient that can be used in labs to make meth.
The medicine, which is recommended in 10 milligram doses every four hours for temporary relief, works by shrinking the dilating blood vessels in the nose, relieving nasal and sinus congestion.
Studies show it works in nasal spray form, but when taken orally, only a miniscule amount reaches the bloodstream, making it ineffective.

In 2007, pharmacy professors at the University of Florida put forth a petition pressing the FDA to review whether a 10 milligram phenylephrine pill worked as a decongestant.
A series of studies pointing to its ineffectiveness have come out since then.
In 2015, a study sponsored in part by the New Jersey-based pharmaceutical company Merck & Co found the the 10 milligram dose, as well as 20, 30, or 40 milligram doses were ‘not significantly better than placebo at relieving nasal congestion’ in a sample of 539 adults.
A few months after that study was published in the Journal of Allergy and Clinical Immunology, University of Florida pharmacy experts launched a second petition demanding the FDA remove the oral medication from the market entirely.
Dr Leslie Hendeles, a pharmacotherapy professor and co-author of the UF petition said in 2015: ‘Scientific evidence continues to show that the most popular products on the market containing phenylephrine are ineffective.
‘Patients who seek an over-the-counter remedy should get what they pay for: an effective and safe alternative to a prescription drug.’

The FDA is seeking public comment on the matter and, if after considering the input, the agency concludes phenylephrine is not effective as an oral decongestant, it will issue a final order removing it from over-the-counter medications.
Following that ruling, drug products would no longer be able to contain oral phenylephrine.
Dr Michele said on a media call Thursday the FDA will ‘provide manufacturers with additional time to either reformulate or remove’ their phenylephrine-only products from the market.
Following the FDA’s announcement that phenylephrine is ineffective, retail pharmacy giant CVS began pulling popular products with the ingredient from its shelves.
Dr Theresa Michele, director of the Office of Nonprescription Drug Products in CDER, said: ‘Consumers should know that a range of safe and effective drugs and other treatments is available to temporarily relieve congestion symptoms due to allergies or a common cold.
‘Consumers can also talk to their doctor or pharmacist about ways to treat these symptoms.’

